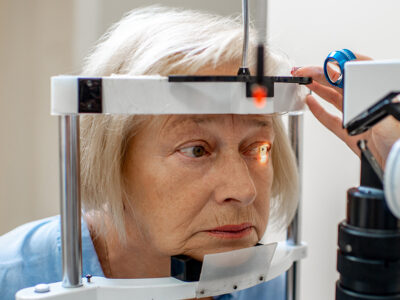
As we age and enter new phases of life, we change direction and focus on personal goals, enjoy new experiences, take up hobbies or sports, and make travel plans to exciting places. Of course, age also introduces us to new health worries. You may think of the typical aches, pains or diminished bodily functions, but many don’t consider eye health. […]
Uncategorized


Be Kind To Your Kidneys
There are multiple health observances celebrated in March. One of them is National Kidney Month. Our kidneys play an important role in our overall health and well-being, so we should give them a little love and attention once in a while. Let’s learn more about how your kidneys function to keep you feeling your best and how you can help […]


Elevating Awareness Of Eating Disorders
The American Psychiatric Association defines eating disorders as behavioral conditions characterized by severe and persistent disturbances in eating behaviors and associated distressing thoughts and emotions. This year, National Eating Disorders Awareness Week is February 20-26. The observance serves as a time to learn more about these disorders and to support the people who suffer from them. Eating disorders are serious […]


Common Childhood ENT Disorders
According to the American Academy of Otolaryngology, ear, nose and throat disorders are one of the main reasons children see a physician. And ear infections are the most common reason parents bring their children to the doctor. February is Kids ENT Health Month, so this blog reviews a few of the more common ENT disorders that affect children. Just about […]


Here’s To Your Heart
February, not suprisingly, is American Heart Month. The human heart is about the size of a clenched fist and weighs between 8 and 12 ounces, depending on gender and body size. Heart disease is the leading cause of death in the United States, killing more than 600,000 Americans each year. That’s one out of every four deaths. There are many […]
Some Thoughts On The Thyroid
The thyroid is a small, butterfly-shaped gland measuring about 2 inches across at the base of the neck. Its sides, or lobes, lie on either side of the windpipe and are connected by a strip of tissue called an isthmus. The thyroid manufactures hormones that control metabolism, the process by which the body changes food and drink into energy. The […]
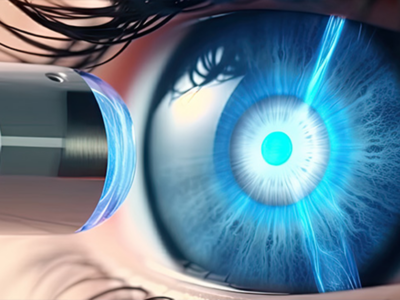
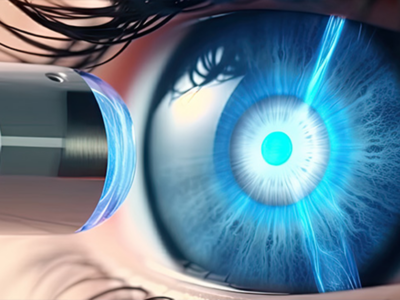
A Glimpse at Glaucoma
Glaucoma refers to a group of progressive eye diseases that cause vision loss by damaging the optic nerve in the back of the eye. The optic nerve is a bundle of more than 1 million nerve fibers that carry messages from the retina, where light is converted into nerve impulses to the brain. The brain interprets the impulses as visual […]


The Basics of Blood Donation
National Blood Donor Month has been observed every January since 1970. It serves as a yearly reminder of the need for blood donations. According to the American Red Cross, someone in the US needs blood every two seconds. If you donate blood you can save a life, or several lives if your blood is separated into its components: red blood […]


A Snapshot Of Cervical Health
Happy New Year! Let’s start off 2023 by delving right into a January health observance: Cervical Health Awareness Month. This observance was created to encourage women to be more attentive to their cervical health and also to learn more about some of the disorders that can affect the cervix. We’ll describe three of those disorders in this blog. The […]


Hand(y) Tips For Staying Healthy
We all know that bacteria and viruses, including the coronavirus that causes COVID-19, trigger infections that can be serious and even life-threatening. These germs are easily spread when you touch contaminated objects or surfaces and then touch your nose, mouth or eyes, where the malicious microbes can enter your body and make you ill. Consider all the objects you touch […]