

Jordan Pysz / iFoundMyDoctor.com
“ I’m going back to Dr. Mavrofrides for sure because I trust him and his team.” – A.J.
When A.J. Rohe was in grammar school, his classmates told him he was good at arguing his case. That talent suits him well in the occupation he selected as an adult. “I’m a divorce attorney,” A.J. relates. “I’ve been in practice since 1997 and own a law firm with several offices in Central Florida. My favorite part of the job is the strategy involved. I like helping people out of the worst situation in their lives and figuring out paths through it to give them the best head start on their new lives.” But law wasn’t A.J.’s first choice of profession. “My undergraduate degree is in philosophy, but I realized that I wouldn’t get paid much as a philosopher, so I took the law school admissions exam and did very well on it,” A.J. recalls. “Still, I wasn’t set on being an attorney. I applied to the University of Florida thinking, If I don’t get accepted, then law isn’t in the cards for me. But I was accepted and enjoyed it. “I got into divorce law because I needed a job after school and the offer was in the county where I grew up. I had a family, student loans and so forth, so even though divorce wasn’t an area of law I wanted to practice, it was a job that I came to love.” A.J.’s professional life has been prospering since he began practicing law 23 years ago, but his personal life took a turn for the worse in February, when an alarming issue developed with the vision in his right eye. The problem grew worse until A.J. was nearly blind in that eye. “I began experiencing symptoms with my eye that I didn’t take seriously because I was having a busy week,” A.J. admits. “First, I started seeing flashes of light in the corner of my right eye, but I figured that was a temporary thing. “The next day, I saw little black dots floating around in my field of vision. I still didn’t take it seriously because they disappeared later that day and into the next day. Then, the dots turned clear and looked like raindrops flowing down a windshield. But I could still see shapes where the dots had been. At that point, I thought I was improving. “The day after that, I saw a little black semicircle in the bottom corner of my eye. While I was in court, the semicircle grew from the bottom corner across the middle of my eye toward the top until I could only see a little bit of light out of the top of my eye.” With the vision in his right eye almost totally obstructed, A.J. finally took his symptoms seriously and went to the emergency room. There were no eye specialists on staff at the ER, so A.J. was advised to contact his general eye doctor, who referred him to Florida Retina Institute. At Florida Retina Institute, A.J. was evaluated by Elias C. Mavrofrides, MD, a board-certified, fellowship-trained retina specialist. After an evaluation and diagnostic testing, Dr. Mavrofrides determined that A.J. suffered a retinal detachment, the peeling away of the retina from the back wall of the eye.
Sticker Shock
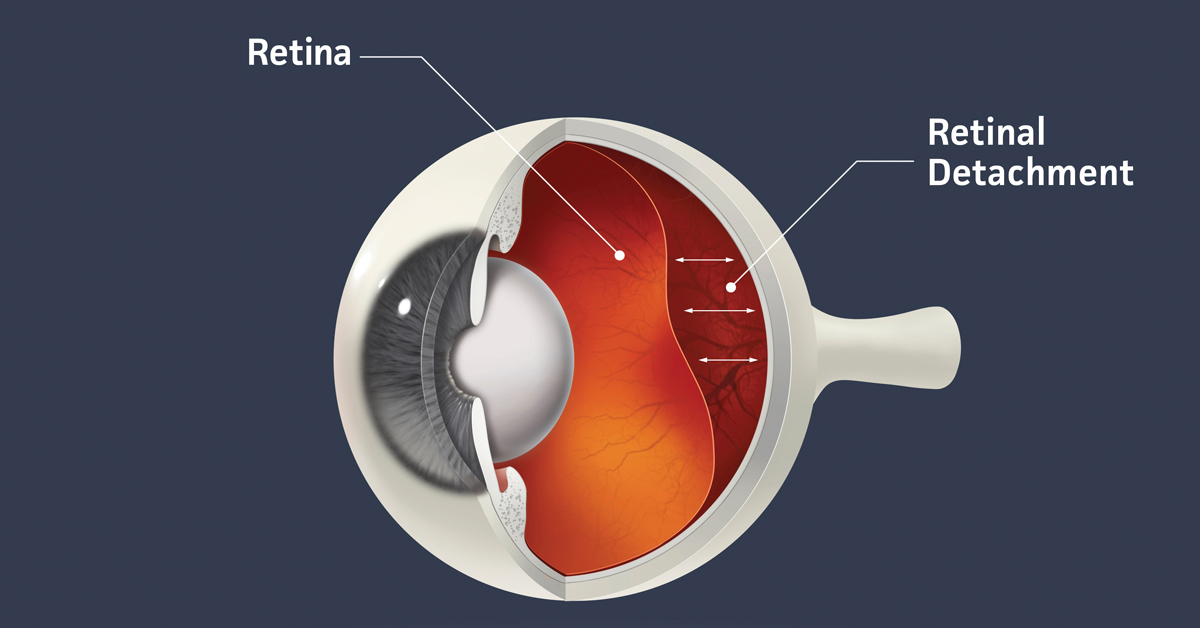
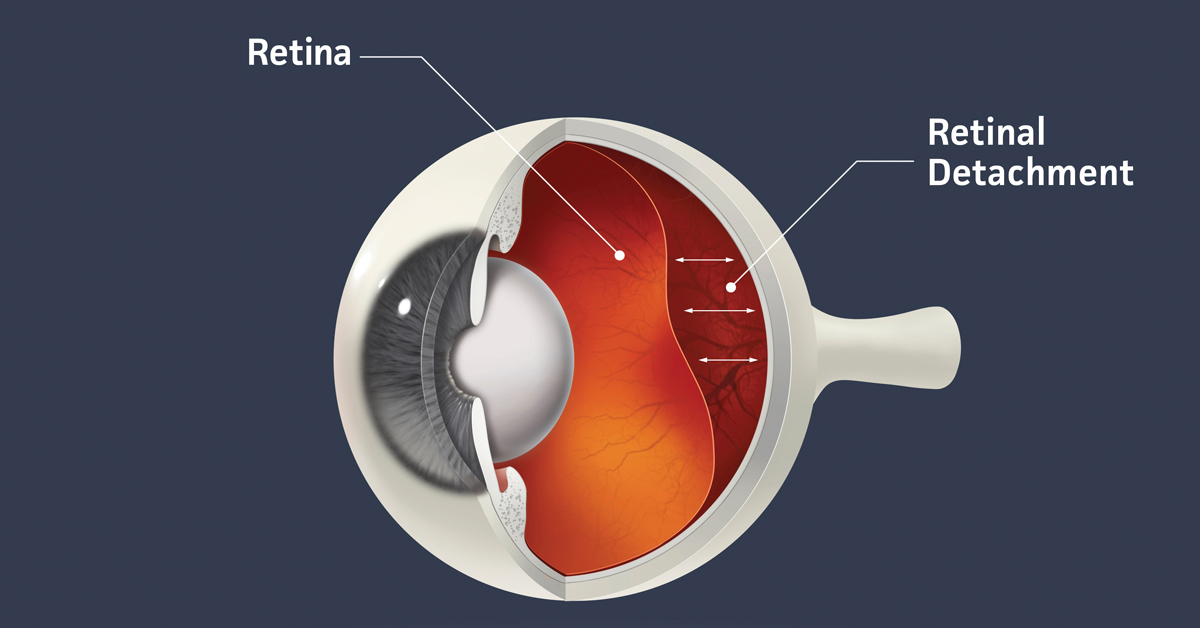
A retinal detachment occurs when the retina, the light-sensitive tissue at the back of the eye, is pulled away from the eyewall. Retinal detachments develop as a result of natural aging changes within the gel, or vitreous, of the eye, Dr. Mavrofrides asserts. “As people get older, the vitreous becomes more liquid and starts to move around the back of the eye,” the retina specialist explains. “At some point, the vitreous becomes so liquid that it actually peels off the retina like a sticker peeling off the skin. “With the vast majority of people, this does not cause a problem. But in a small percentage of people and for reasons we do not understand, the vitreous pulls on the retina during this process, causing a tear in the retina. And a tear enables the retina to detach because fluid leaks through the tear and peels the retina out of place.” An obstacle to detecting retinal tears and detachments is that they have few obvious symptoms. Typically, there is no pain or discomfort when the detachment occurs. During the beginning phases, people may notice flashes or floaters in their field of vision, which can signal that the vitreous is peeling away the retina. But not all eye floaters are related to retinal tears and detachments. “Some people may notice a shadow or curtain falling over their peripheral vision,” Dr. Mavrofrides adds. “Retinal tears usually develop in the far edges of the retina, which is associated with peripheral vision. As fluid accumulates and the retina detaches, problems with vision shift toward the central vision. “The main diagnostic tool for retinal detachment is the dilated retinal exam in which we use a special light and lens to examine the back of the eye and determine the position of the retina. We also use the ultra-wide-field OPTOS® Imaging System that provides an extremely detailed view of the retina for diagnostic purposes.”
Bursting Bubbles
There are several options for treating retinal detachment. One is an in-office procedure called pneumatic retinopexy. “During pneumatic retinopexy, we inject a special gas bubble into the eye to push the retina back into position and reattach it,” Dr. Mavrofrides describes. “This procedure can only be performed if the detachment is located on the upper edge of the retina.” Pneumatic retinopexy is the only treatment for retinal detachment that can be offered in a clinic setting. All other options are performed in an operating room or surgery center. “The main surgical procedure for retinal detachment is vitrectomy in which we remove the vitreous gel, reattach the retina internally and use a laser to seal the retina into place,” Dr. Mavrofrides informs. “During vitrectomy, we also inject a gas bubble to help hold the retina in place as the gluing effect of the laser takes hold. The gas bubble remains in the eye temporarily while the retina heals. Unfortunately, it tends to block vision, causing obstructed vision for two to four weeks after surgery. But in time, the body absorbs the bubble, the eye fills with its own fluid and vision improves. “A third surgery, called a scleral buckle, is the oldest treatment for retinal detachment,” Dr. Mavrofrides continues. “During this procedure, we sew a special band, which is like a belt, around the eye to pinch together the wall of the eye and the retina. Scleral buckle is less common nowadays and generally only performed in certain situations.” A.J. was given a choice of the in-office procedure or the vitrectomy performed in a surgical center. Based on Dr. Mavrofrides’ explanation of the two and the odds of success, he chose the latter. “Dr. Mavrofrides said there was an 80 percent chance of success with the in-office procedure versus a 90 percent chance of success with the surgical procedure,” A.J. remembers. “I figured if a 20 percent chance of failure is reduced to a 10 percent chance, I’ve doubled my odds, so I agreed to have the procedure at the surgery center.”
Jordan Pysz / iFoundMyDoctor.com
“Dr. Mavrofrides performed my surgery with care and precision. He’s a wonderful individual. I’m glad I met him and went through this experience with him.” – Dennis
Mobile Monitoring
Before retiring a year ago, Dennis Hoar was self-employed for more than 30 years. He owned an environmental compliance company that inspected clients’ fuel supplies and tanks for leaks and kept clients up to date with local, state and federal regulations. “The job involved visiting client sites and making sure their tank levels were accurate and there was no loss of fuel,” Dennis describes. “I also checked that their equipment was undamaged and working properly. There are electronic devices that monitor the equipment, and I’m certified to maintain those devices and replace parts when needed. “For the last 30 of those 32 years I was in business, my primary client was United Parcel Service. I had contracts with UPS out of Jacksonville and Orlando. I inspected the fuel tanks that service the delivery trucks at all the UPS sites in central and north Florida.” Dennis got involved in the environmental compliance business through a friend from his church. At first, the pair performed inspections manually, but the technology soon evolved into electronic monitoring. Dennis returned to school to become a certified electronics technician, and his career – and business – advanced from there. Now retired, Dennis fills his days doing odd jobs and helping friends and family. He also writes poetry as the muse inspires him. Formerly a full-time Gospel preacher, Dennis still takes the pulpit from time to time, and he stays close with his church family. It was his strong faith that sustained him when he faced a serious health threat last year. “It started on December 4, 2019,” Dennis says. “I noticed that I wasn’t able to see anything to my right side in my peripheral vision. Usually, when I look forward, I can see a great deal to the side. But when this happened, I couldn’t do that. It seemed like my eye was closing down on me. When the loss of peripheral vision devolved into a total loss of sight in his right eye, Dennis knew he needed to see an eye specialist. Unsure of what type of specialist to consult, Dennis called the ophthalmic practice he visited several years earlier when he underwent cataract surgery. “When I went to their office, the doctor told me I might be experiencing a detached retina,” Dennis recounts. “She referred me to Florida Retina Institute, where I was examined by Dr. Mavrofrides.” As he did with A.J., Dr. Mavrofrides used a dilated retinal exam and the OPTOS Imaging System to diagnose Dennis’ eye disorder.
“It is a myth that retinal detachments are emergencies and must be treated immediately. … In reality, how quickly a detachment is repaired has very little influence on visual outcomes.” – Dr. Mavrofrides
“Dr. Mavrofrides pulled up my test results and quickly confirmed that my condition was indeed a retinal detachment,” Dennis notes. “My appointment was on a Friday, and Dr. Mavrofrides told me to go to the retina surgery center the following Monday for treatment.” “It’s a myth that retinal detachments are emergencies and must be treated immediately,” Dr. Mavrofrides reports. “Certainly, we want patients with symptoms to contact us for an evaluation as soon as possible but, in reality, how quickly a detachment is repaired has very little influence on visual outcomes. “Actually, visual outcome after retinal detachment is influenced by a tremendous number of factors, many of which are out of our control.” “It’s a scary thing to have surgery on your eyes thinking you could lose your sight as a result, but Dr. Mavrofrides was very comforting and reassuring,” Dennis states. “He prepared me for what I was about to experience. There was virtually no pain or discomfort during the very delicate procedure, and Dr. Mavrofrides did an excellent job.”
Unexpected Consequence
Like A.J., Dennis chose to undergo the vitrectomy. In the case of both patients, the gas bubble caused a temporary vision obstruction, just as Dr. Mavrofrides said it would, but as the body absorbed the bubble, each patient’s vision returned to normal. “During the follow-up appointments after my surgery, Dr. Mavrofrides recognized that I was healing exceptionally well and quickly,” Dennis reports. “During my last office visit on May 28, Dr. Mavrofrides deemed everything a success. “My experience was better than I could possibly have expected. Dr. Mavrofrides performed my surgery with care and precision. He’s a wonderful individual. I’m glad I met him and went through this experience with him. “I used to be a Gospel preacher so I have a great deal of faith. I realize that God worked his blessing in me with my recovery, but Dr. Mavrofrides has my highest appreciation.” Immediately following his vitrectomy, A.J. noticed one positive change in his vision. He could see colors again. But there was a post-surgery complication: the development of cataracts. Dr. Mavrofrides explains that the acceleration of cataract formation is a common consequence of retinal detachment surgery. Dennis had cataracts removed from both eyes before his retina detached; A.J. did not. “A cataract is almost like a doughnut glaze over the eye that’s difficult to see through,” A.J. describes. “It causes light to flare out, which also makes it difficult to see, so I’ll be undergoing surgery soon to remove the cataract. “As for the retinal detachment, it’s been about 3½ months since the surgery, and there’s still some visual distortion, but it’s nowhere near what it was at the beginning. My understanding is that it will continue to improve. “But now, I’m having problems with my left eye. And for that I’m going back to Dr. Mavrofrides for sure because I trust him and his team.”






Leave a Reply