COURTESY PHOTO
As we age and enter new phases of life, we change direction and focus on personal goals, enjoy new experiences, take up hobbies or sports, and make travel plans to exciting places.
Of course, age also introduces us to new health worries.
You may think of the typical aches, pains or diminished bodily functions, but many don’t consider eye health. We accept that eyeglasses, maybe even readers, are part of our everyday life, but little beyond that. However, vision problems, especially glaucoma, are irreversible and can rob you of these long-awaited experiences.
The Centers for Disease Control and Prevention estimates that 3 million Americans suffer from glaucoma and list it as the second leading cause of blindness. A diagnosis of glaucoma can happen at any age, but the chances increase after 60, often gradually with no symptoms.
Glaucoma is a serious disease associated with high fluid pressure in the eyes, or intraocular pressure (IOP). Consistently high IOP can damage the optic nerve and lead to vision loss.
Intraocular pressure is primarily determined by the balance between the production of aqueous humor (a clear fluid within the eye) and its drainage. The eye continually produces this fluid, and it needs to drain properly to maintain a normal pressure within the eye.
The drainage goes through two independent pathways: the trabecular meshwork and uveoscleral outflow pathway, explains Michele McLin, OD, an optometrist in Boynton Beach.
“In patients with glaucoma, fluid inside the eye is not draining properly through these pathways, therefore increasing intraocular pressure on the optic nerve,” Dr. McLin says. “This pressure can cause damage resulting in deterioration of one’s vision.”
Although there is no way to restore vision loss from glaucoma, early detection and treatment can slow it down.
Types And Symptoms
Open-angle glaucoma is the most common, occurring when resistance builds in the drainage pathways. Although the pathways appear to be open and functioning normally, over time fluid can build, placing pressure on the optic nerve. Often, this type of glaucoma has no symptoms, but some may experience headaches, eye pressure, rainbow-colored halos around lights, blurred or narrow vision, red eyes, nausea or vomiting.
Closed-angle, or narrow-angle, glaucoma is rare and often comes on suddenly. It occurs when the angle between the iris and cornea is too narrow and blocks the drainage pathways. The cornea is the transparent part of the eye that covers the front of the eye, including the lens and iris, which is the colored area that has muscles to control the pupil.
With closed-angle glaucoma, patients may experience eye pain or headaches that can be severe and may require medical attention.
Dr. McLin says there are other conditions that can contribute to closed-angle glaucoma, but it is primarily caused by disorders of the iris, lens and structures behind the lens.
Normal- or low-tension glaucoma is optic nerve damage occurring when pressure is not elevated. Nearly one in three people have this condition and experts are uncertain about the cause, although it is more common among people of Asian descent. Most patients do not have symptoms.
Congenital glaucoma results from drainage canals not forming properly in utero. A health care provider may observe glaucoma symptoms at birth or during childhood. Symptoms may include light sensitivity, hazy gray cornea, enlarged eye or cornea, an overflow of tears, or vision loss.
“Systemically, health conditions such as sleep apnea have been linked to the development of glaucoma,” Dr. McLin states. “Studies have shown that diabetes, heart disease and blood pressure can also have correlations to glaucoma, though their exact mechanisms are not clear.”
-Dr. McLin, OD, South Florida Vision


COURTESY GRAPHIC
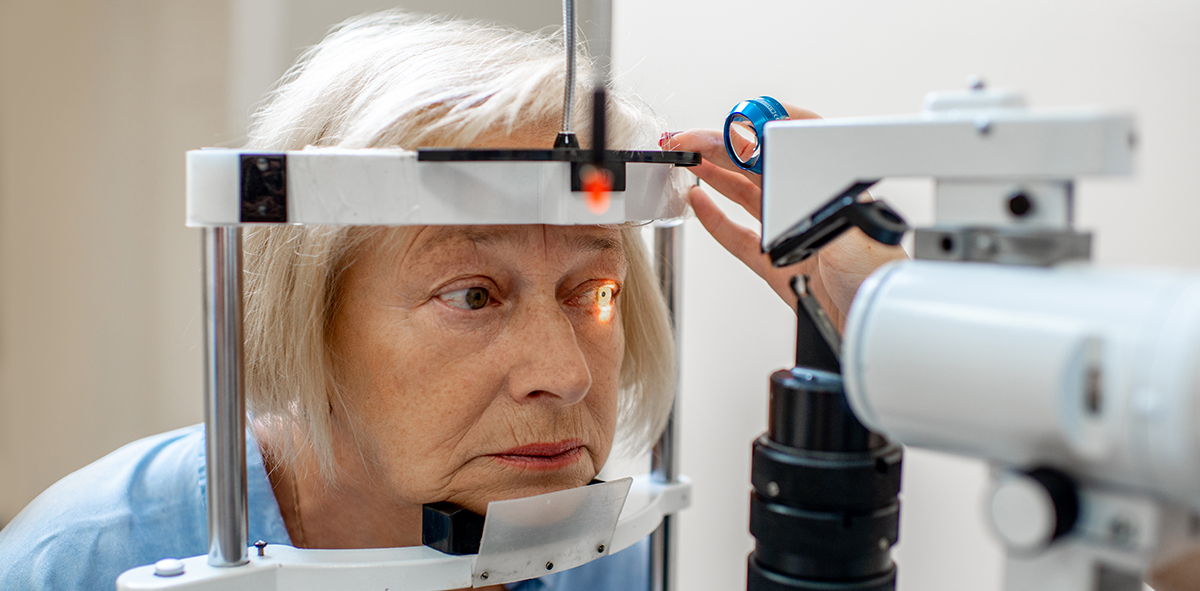
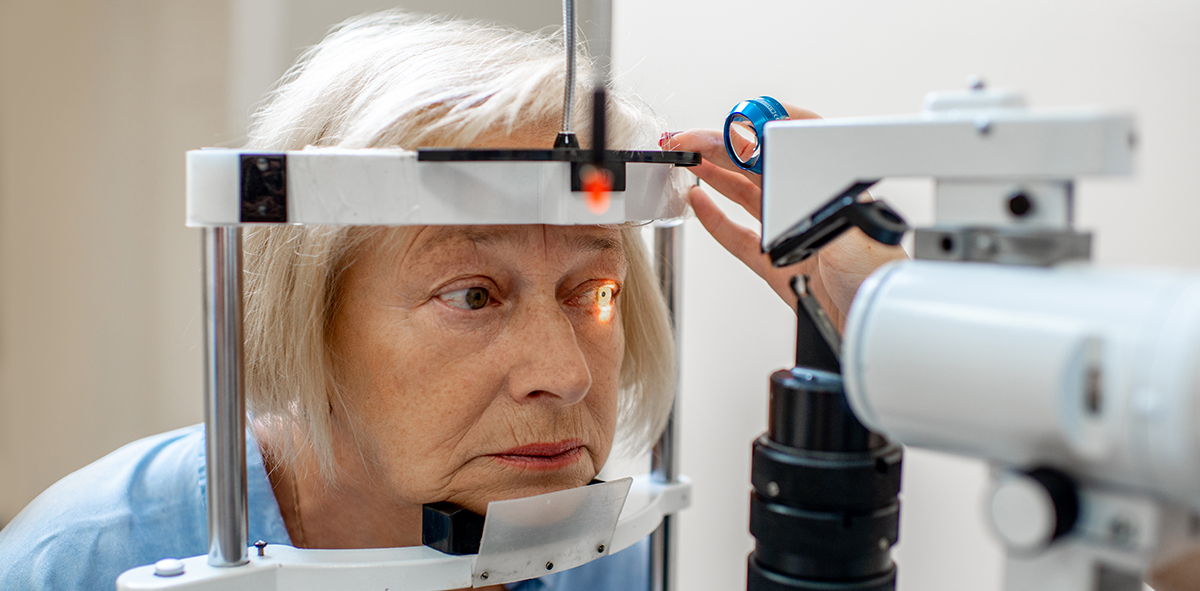
Diagnosing Glaucoma
Regular eye exams are critical in early diagnosis of glaucoma. An optometrist or ophthalmologist may also do one or more of the following:
- Dilated eye exam to view the optic nerve and back of the eyes.
- Gonioscopy, a test that uses a special lens and slit lamp to determine the drainage angle of the eye.
- Optical coherence tomography (OCT) to look for changes in the optic nerve.
- Ocular pressure measurement.
- Pachymetry to measure corneal thickness.
- Evaluate for vision loss through various tests.
- It is important to consult with your health care provider and/or eye doctor if you experience eye pain, severe headaches or vision problems.
Managing And Treatment
There is no cure for glaucoma, but early diagnosis, regular eye exams and some treatments can assist in reducing the speed at which vision loss occurs.
“There is nothing preventative that can be done to stop the likelihood of developing fluid buildup on the optic nerve,” states Dr. McLin. “Genetics can put you in a higher risk class for developing glaucoma, but it is not definite. Just because Mom has glaucoma, does not mean you will. It just raises your risk.
“Yearly eye exams with your optometrist include monitoring eye pressure to check for any increases or changes in fluid pressure. If changes are noted, treatment can be initiated.”
Topical ophthalmic agents (eyedrops) are often the first line of treatment for glaucoma. There are numerous classes of medication.
Some help drain fluid to reduce eye pressure, such as latanoprost (XALATAN®), tafluprost (ZIOPTAN®) and bimatoprost (LUMIGAN®). Others lessen the amount of fluid the eye makes, including timolol (TIMOPTIC®) and dorzolamide (TRUSOPT®).
Your provider can determine which is best for your diagnosis.
In 2020, the FDA approved a bimatoprost implant (DURYSTA®) to reduce intraocular pressure. It was the first sustained-release therapy for glaucoma. When placed in the eye, the biodegradable implant releases medication over three to six months.
“Clinical trials have demonstrated that a bimatoprost sustained release implant can provide comparable levels of intraocular pressure control as topical eyedrops,” explains Dr. McLin.
“Bimatoprost advantages include: decreasing concern over adherence to eyedrop administration, reducing ocular surface and periocular side effects from topical drops and decreased daily treatment burden on patients.
“Additionally, studies have shown continued lowering of eye pressure over extended follow-up periods even after all the medication has been delivered.”
Laser treatment may also be an option to help improve drainage. It may be used alone or in conjunction with eyedrops. In some situations, laser treatments can last for a few years.
Surgery can be used to quickly reduce eye pressure by improving drainage or reducing aqueous production. There are several options, including minimally invasive glaucoma surgery, or MIGS. Patients should discuss these options with their eye doctors.




Leave a Reply