

Pain is a subjective sensation. A level of pain that one person considers tolerable may be deemed excruciating or even disabling by another. It’s no wonder that treating pain, especially chronic pain, has proved to be so challenging.
Though everyday scrapes, bumps and bruises can usually be treated rather effectively with over-the-counter or even home remedies, a safe, effective answer for the kind of aggravating pain that slows someone for weeks, months or even years remains elusive.
The proof is in the numbers.
According to a study conducted a few years ago by the National Institutes of Health, approximately 50 million people in the US suffer from what medical professionals describe as chronic or severe pain.
That’s more than twice the number diagnosed with diabetes, more than three times the number treated for cancer and nearly twice the number known to have heart disease, the NIH states.
Figures such as those are why chronic pain is considered to be an epidemic and why practices such as Jax Spine & Pain Centers remain committed to finding better ways of safely and effectively treating chronic pain.
With offices in Jacksonville, St. Augustine, Fleming Island and Fernandina Beach, Jax Spine & Pain Centers specializes in progressive interventional treatment options for pain. It is also committed to combatting the use and overuse of opioids. As part of that venture, it offers a leading-edge treatment for pain that most other practices don’t.
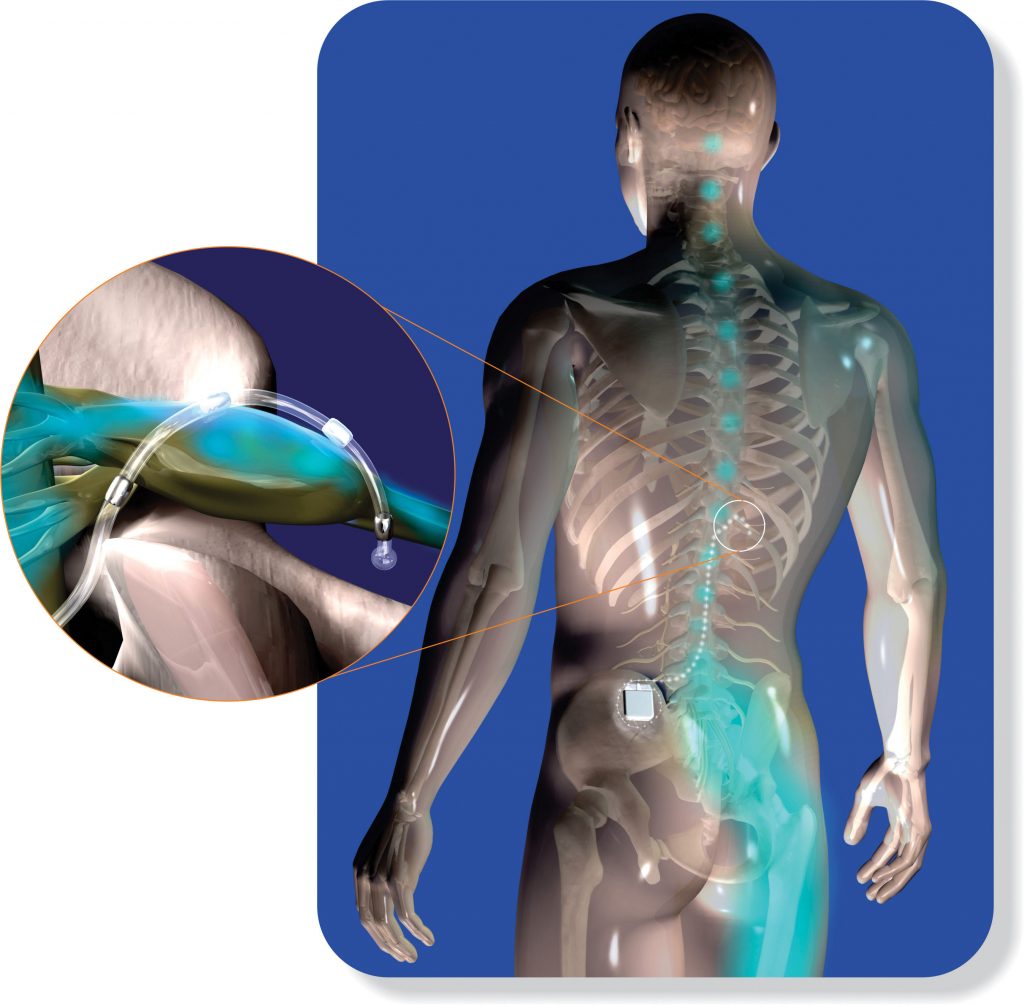
That treatment is called DRG stimulation. It is an advanced form of spinal cord stimulation, a decades-old remedy for chronic pain in which electrical impulses keep pain messages from traveling to the brain.
By interrupting these messages, the stimulus for pain is not detected, so less pain is felt by the individual. DRG stimulation is a byproduct of the older therapy that allows for the treatment of pain in isolated areas of the lower body.
“DRG stimulation has been around only for about three or four years, but it’s become more mainstream in the last year as more practitioners have become aware of it and have been trained on it,” confirms Claudio Vincenty, MD, of Jax Spine and Pain Centers. “The advantage is that we can target and treat one specific area of the body with it.
“For example, we have a patient who had an amputation and was experiencing phantom limb pain at the point where his leg was amputated. With the old stimulation system, we would have had to provide stimulation in the middle of the spinal column that would have impacted the entire leg. With DRG stimulation, we can target only the nerves that go to the painful part of the leg.”
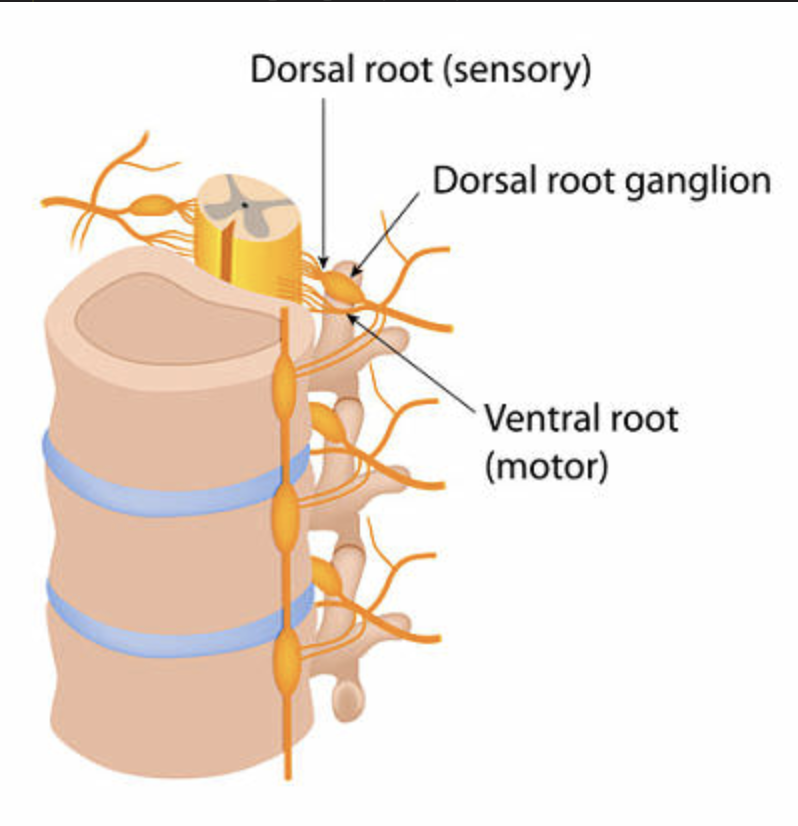
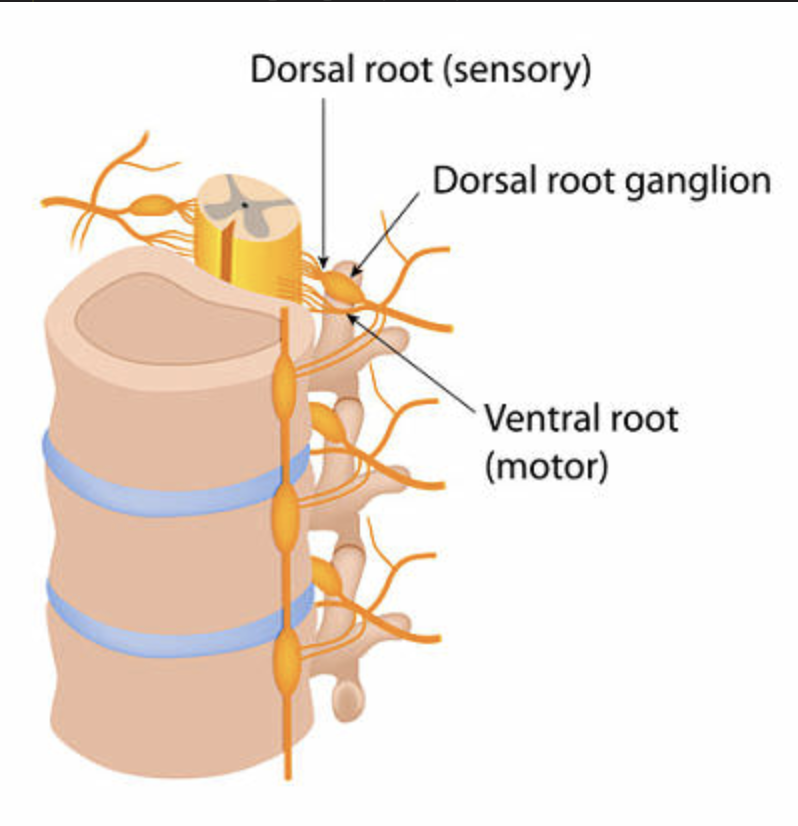
DRG stimulation does this by affecting the dorsal root ganglion (DRG), which are the cell bodies of sensory neurons that control pain signals. The DRG are located at the side of the spine where the spinal nerve root exits to become a peripheral nerve.
This ability to treat specific areas of the body where pain is experienced is something researchers have sought for decades. The discovery is being celebrated throughout the medical community.
“DRG stimulation is, in essence, the Holy Grail of spinal cord stimulation,” states Justin D. Mann, MD, of Jax Spine & Pain Centers. “It’s something that’s been in the works since spinal cord stimulation was first used way back in the 1970s.
“Prior to discovering DRG stimulation, the areas of the body we could treat through stimulation were very broad. This is a much more targeted therapy that allows us to provide substantial pain relief that gets people feeling better and back to living their life.
“Think of it this way: If you can put a hand on the area that hurts, and your pain is limited to that area, then DRG stimulation is going to be very effective in treating that pain. That’s how targeted it is.”
Addressing Nerve Damage
DRG stimulation is used primarily in the treatment of chronic nerve pain in the lower body – the hips, knees, ankles and feet. It is also used to treat causalgia, which is chronic pain that develops following an injury or an event such as a stroke or heart attack.
Often referred to clinically as complex regional pain syndrome, or CRPS, causalgia is characterized by abnormal inflammation or nerve dysfunction and pain greater than that experienced during the suffering of the injury that caused it.
For example, someone might experience a severe knee injury that requires surgery or undergo surgery for a hernia. However, pain in the region persists weeks or even months afterward, often because nerves are often damaged during surgery. Studies show that between 10 and 40 percent of patients undergoing surgery endure some sort of post-surgical neuropathic pain.
That is especially true with amputations and paralysis, but doctors have found that people with severe diabetes as well as women who gave birth through cesarean section suffer with nerve pain for months or years.

This pain is sometimes a result of nothing more than a scarring of the nerves, but the scar tissue in scarred nerves can compress a nerve in a way that limits the nerve’s ability to be fed the natural elements that allow it to remain healthy.
In addition to pain, damaged nerves can cause numbness, tingling, burning, muscle weakness and atrophy. When those symptoms last longer than a few months, they are considered permanent and in need of treatment.
First Things First
“Treatment of such pain problems typically begins conservatively,” states Nicholas Bremer, MD, of Jax Spine & Pain Centers. “There’s a process we follow that starts with medications, physical therapy or maybe steroid injections. If that doesn’t work, we typically try something more advanced, like ketamine infusions or peripheral nerve blocks. But if you’ve tried all of that and nothing has helped, it usually leads to nerve stimulation.”
As with spinal cord stimulation, DRG stimulation starts with a five- to seven-day trial that begins with the doctor threading two small catheters the width of a strand of spaghetti into the epidural space of the spine.
“We perform this procedure in our office, and it’s done while the patient is under light sedation,” states Michael Hanes, MD, of Jax Spine & Pain Centers. “Sometimes we can even get away with just having the patient take a Valium®.”
The catheters contain leads or electrodes that are placed on the dorsal root ganglion. The spinal column contains several ganglia, each of which is associated with a different area of the body. Physicians know which DRG to stimulate based on the location of the pain.
“These areas are pretty well mapped out, although there can be some variation from person to person,” Dr. Hanes educates. “That’s why we have a trial of the system first, without incisions, and just using needles to place the leads.”
The other end of the electrodes are connected to an external device that creates electrical impulses that block the body’s painful pathway. The pain can be replaced with either a gentle tingling or no sensation at all.
“The device that the bottom ends of the leads are attached to is an externalized pulse generator,” Dr. Bremer details. “It’s a combination battery and pulse generator, and for the duration of the trial, that device is taped to the patient’s back.
“The patient goes about normal daily activities about five to seven days to see how effective the treatment is in relieving pain. If it’s effective, we move ahead to placement of the permanent DRG stimulator.”
Remote Control
During the trial period, patients can control the amount of stimulation they receive by using a remote control that allows for different programs to be locked into it. The remote control also allows the patient to turn the device on or off as needed.
At various points during the trial, the patient will likely be contacted by the doctor or a representative of the device’s manufacturer to see how the trial is going. At the end of the trial, the patient and doctor meet again to discuss the patient’s experience.
“If it didn’t go well, meaning they failed to experience significant pain relief, then we simply remove the leads, knowing that we did as much as we could in that regard,” Dr. Bremer reports. “In those cases, we explore other options.
“But for those who do experience pain relief, and that is the case with a majority of the patients who complete the trial, we move on to get insurance approval for placement of the permanent device.”
To gain approval, a patient must experience a reduction in pain and an increase in function of between 50 and 80 percent. That reduction is measured using a visual analog or numerical scale.
“There are many types of pain and disability scales out there, including some that measure not just pain and function but emotional things as well,” Dr. Bremer educates. “We use different scales, but in general, we’re asking, Did this help you, and if so, how much?”
The implant procedure is similar to the one used for the temporary device, except that it takes place at an outpatient surgery center.
“In that setting, the patient is put to sleep and we implant the system underneath the skin, usually in the flanks,” Dr. Mann discloses. “When the patient wakes up, the system is in place and it gets programmed over the coming days and weeks.”
Longer Lasting Battery
The battery powering the system is a technological marvel in and of itself. According to the doctors at Jax Spine & Pain Centers, the battery can maintain a charge for at least seven years and in some cases up to 10 years.
“With the more traditional devices, patients would have to recharge the battery every couple of weeks or so,” Dr. Vincenty notes. “But as it is with almost everything these days, the technology in the battery has improved tremendously.”
Dr. Hanes adds: “The fact that you hardly ever have to charge the device is one reason this is considered a very convenient therapy. Another is that you don’t feel the stimulation. It’s always running but you don’t know it’s there.”
The patient will know it’s working by the reduction in pain it provides. According to the team at Jax Spine & Pain Centers, most patients who have received the DRG stimulator report a reduction in pain of at least 50 percent.
“Among my patients, it’s somewhere in the neighborhood of 85 to 90 percent received enough relief from it to have the permanent system implanted,” Dr. Mann reveals. “So, it’s an effective treatment that we are thrilled to provide.”











Leave a Reply