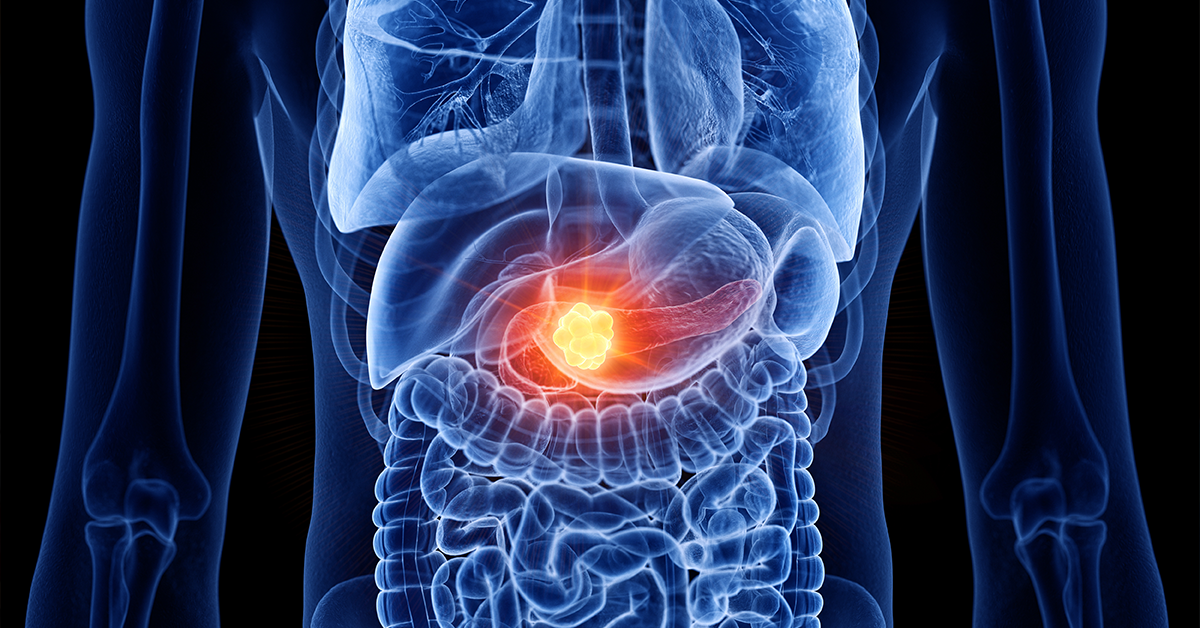
November is Pancreatic Cancer Awareness Month, so let’s take a few minutes to ponder this deadly disease. First, let’s learn a little bit about the pancreas and its important contributions to the body’s day-to-day functioning.
The pancreas is an oblong organ that sits across the back of the abdomen, between the stomach and the spine. It consists primarily of two types of cells. Exocrine cells make key enzymes for digestion, which they release into tiny tubes called ducts. Endocrine cells produce hormones such as insulin and glucagon, which help the body absorb glucose (sugar) for energy and control glucose levels in the blood. Endocrine cells release their hormones directly into the bloodstream.
Pancreatic cancer develops when abnormal cells grow out of control and form a mass, or tumor. About 95 percent of pancreatic cancers start in the exocrine cells. These are called pancreatic adenocarcinomas. About 7 percent of pancreatic cancers begin in the endocrine cells. Those are called pancreatic neuroendocrine tumors, or PNETs.
According to the American Cancer Society, pancreatic cancer accounts for about 3 percent of all cancer diagnoses in the US and is responsible for 7 percent of cancer deaths. The society estimates that about 62,210 Americans will be diagnosed with pancreatic cancer in 2022 and about 49,830 people will die from it.
Pancreatic cancer is often called a “silent cancer” because it generally has no detectable symptoms in early stages. Consequently, it typically progresses and affects other organs and tissues before it is diagnosed.
When present, pancreatic cancer symptoms can include yellowing of the skin or eyes (jaundice), dark urine, pain in the abdomen or lower back, digestive upset (nausea, vomiting or indigestion), fatigue, depression, blood clots, decreased appetite, unexplained weight loss and sudden onset of diabetes.
The cause is unknown, but certain factors have been identified that increase the risk for developing this cancer. These include smoking cigarettes, being obese, not exercising regularly, eating a diet high in fat and processed meats, drinking heavily, being exposed to chemicals and pesticides, having Type 2 diabetes or a chronically inflamed pancreas, being African American, being male, being older than 55 and having a family history of pancreatic cancer.
To diagnose pancreatic cancer, a doctor will begin with a thorough review of the patient’s symptoms and medical history. The doctor will likely order a CT or MRI scan to get a detailed image of the pancreas. Other tests may include endoscopic ultrasound and endoscopic retrograde cholangiopancreatography (ERCP).
These tests are performed through an endoscope – a thin, flexible tube with a tiny camera attached to its end that is passed down the throat and into the digestive system. During these endoscopic procedures, a doctor can obtain a sample of tissue to study under a microscope to look for cancer cells. This is called a biopsy.
Blood tests are also used to look for certain tumor markers that may indicate pancreatic cancer. Tumor markers are substances that are often found in high concentrations when cancer is present. Tumor marker CA 19-9 may be helpful in diagnosing pancreatic cancer. Carcinoembryonic antigen (CEA) is another tumor marker for pancreatic cancer, but it’s not used as often as CA 19-9.
Once a diagnosis of pancreatic cancer has been made, the doctor will assign a stage based on test results. The stage of a cancer indicates the size of the tumor and how far it has spread from where it originated. The stages of pancreatic cancer include:
• Stage 0 – Abnormal cells that could become cancerous are present in the pancreas.
• Stage 1 – Tumors are in the pancreas only.
• Stage 2 – Tumors have spread to nearby abdominal tissue or lymph nodes.
• Stage 3 – The cancer has spread to major blood vessels and lymph nodes.
• Stage 4 – The cancer has spread to other organs, such as the liver.
Treatment for pancreatic cancer depends on the stage. The goals of treatment are to kill the cancer cells, prevent the spread of the disease and relieve symptoms. Treatment may include surgery, chemotherapy, radiation therapy, targeted drug therapy and immunotherapy.
If the cancer is localized to the pancreas, it may be possible to eliminate the cancer cells by surgically removing all or part of the pancreas. A common procedure for pancreatic cancer is the Whipple procedure during which the surgeon removes the head of the pancreas and sometimes the entire pancreas, along with a portion of the stomach, the first part of the small intestine, the gallbladder, the bile duct and other tissue.
Chemotherapy uses drugs to kill cancer cells. Radiation therapy destroys cancer by focusing high-energy rays on the cancer cells. These treatments may be used before surgery to shrink tumors or after surgery to eliminate any remaining traces of the cancer.
Targeted drug therapy is a type of cancer treatment that targets proteins that control how cancer cells grow, divide and spread. Immunotherapy works the immune system to recognize and destroy cancer cells.
Because pancreatic cancer is typically not diagnosed until it is in its advanced stages, it continues to be difficult to treat and cure. Fortunately, the outlook for people with this cancer is improving. Ongoing research and clinical trials, along with new treatments, are expanding the average five-year survival rate for people with pancreatic cancer.




Leave a Reply